The New Omicron Booster and Flu Season Have Pushed Pharmacy Workers to Their Limit - The New Republic
Days before the new omicron-specific bivalent Covid booster was rolled out at her Walgreens store, Salem, a pharmacy operations manager who works near Chicago, received word from Corporate that the vaccines were on their way. "We were told Thursday that week would be the earliest," she said. "Suddenly we received a shipment of two boxes that Monday."
The first day wasn't so bad—only one patient realized the new vaccine was available. But the following day, "chaos ensued," she said. Shots were scheduled every 15 minutes from 9:30 a.m. to 6:15 p.m., with no breaks. "That first day, we didn't even know how many milliliters the patient was to receive in the shot," she said. "We didn't know if it was OK to give with a flu vaccine. We didn't know if it had any side effects. We didn't even know how to properly post the vaccine to our inventory system."
Pharmacists also felt the pressure in the early days of the new vaccine rollout. As Matt, a pharmacist and manager at a retail pharmacy near Tucson, Arizona, said, "As the new omicron boosters roll out, the extreme anxiety has returned"—worsened by his company's requirement that pharmacies accommodate walk-ins at all hours of the day.
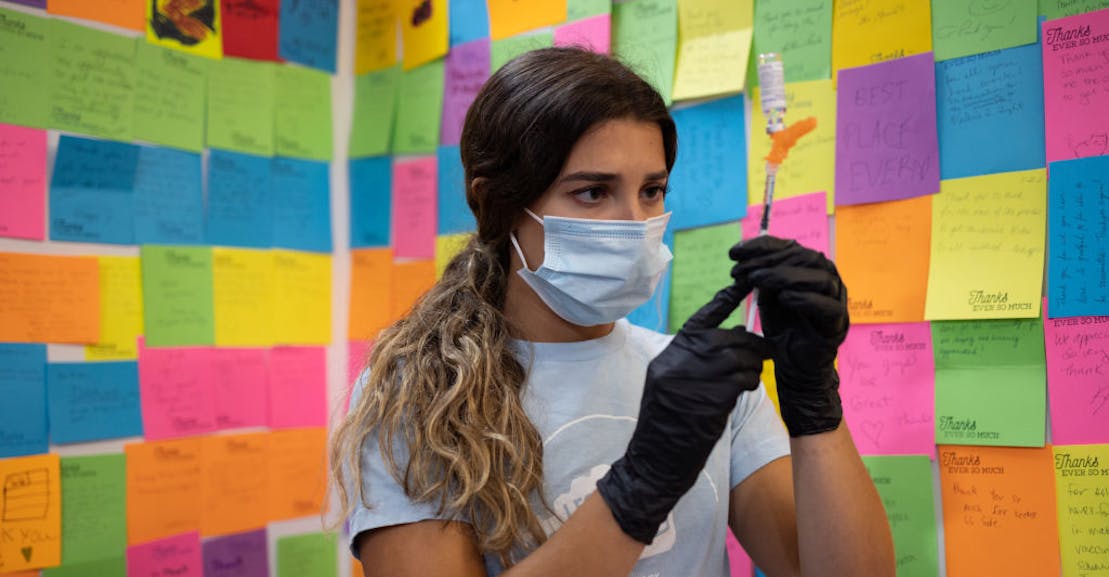
Making matters more dire, the new vaccine rollout coincides with flu season, typically the busiest time of year at the pharmacy. And beyond public health, retail pharmacy chains like CVS and Walgreens—which are publicly traded companies raking in tens of billions in profit per year—have huge financial incentives to vaccinate as many people as possible. The problem is, they're essentially adding an additional job for workers who are already spread too thin. As corporate expectations grow, patient care—and pharmacy workers' sanity—suffers.
The pandemic has exacerbated preexisting labor problems in the pharmacy field, while also offering a financial boon for the corporations. Yet as pharmacists' and other pharmacy workers' workloads and responsibilities have increased, their pay has stagnated, as they've faced increased pressure and stress from corporate managers to give more shots, more quickly, no matter the consequences. At least during initial vaccine rollouts, government-run supersites staunched the deluge. But states have largely closed down those sites, and pharmacies now bear the brunt of vaccinating the nation.
"I was all for pharmacists being able to vaccinate America, because we were well-positioned to do so," said Shane Jerominski, a pharmacy manager at an independent pharmacy in Southern California. "But we weren't given the resources to be able to do that and to also do our other job, our primary job, … the safe and accurate dispensing of medications."
Salem said that at her Walgreens location, over 100 prescriptions need to be filled at any given time. Of those, over half have insurance issues and a third are out of stock, or only part of the month's pills are available. Meanwhile, they're scheduled to step away from the counter to give shots every 15 minutes—and in some cases, more frequently.
"It is not uncommon to work 14 hours without a break to eat, pee, or even drink much water," explained Alex Evans, a pharmacist and medical writer who decided to take a "midcareer break" last year. Now he's not so sure he'll go back. "I take every opportunity I get to steer people away from pharmacy," he said.
According to a 2021 study, some 75 percent of pharmacists are burnt out. "Some days you're just clinging on, feels like a fog, then driving home hoping you didn't miss or cause any drug errors today," said Paul, a pharmacist in Columbus, Ohio. The consequences of these mistakes can be dire. Pharmacists "can't spend time talking to their patients, they feel like patient care is suffering, and they often even feel like patient lives are being put at risk," added Evans.
Now, in addition to vaccination demands, retail pharmacies are making an effort to allow pharmacists to dispense Paxlovid, the Covid antiviral therapy. Pharmacists are torn about this: On the one hand, many support making this treatment more available and being able to bill for the service they're providing. On the other hand, pharmacists aren't sure they have the time or ability to prescribe it safely. Paul said that his first Paxlovid prescription took him two hours, "from talking to the patient, reading their profile, and then actually having a discussion with the physician, and ultimately approving the prescription to go out to the pharmacy. And nobody is being compensated for that either."
CVS's Paxlovid program is underway at select locations: To be eligible, patients who have tested positive for Covid-19 must fill out an online screener, then schedule a phone call with a pharmacist, and then, if approved, pick up their prescription at a drive-through location or have it delivered. Fraser Engerman, a spokesperson for Walgreens, confirmed that the company is also piloting a program in Kentucky and Florida where pharmacists are able to prescribe and dispense Paxlovid to eligible patients.
While pressing pharmacists to take on even more responsibility, corporate retail chains are also holding them to metrics to reach sales goals and quotas. Though Engerman denied that Walgreens enforces "sales goals or quotas for Covid vaccines or any other pharmacy service," there are numerous reports to the contrary.
"In chains, I would absolutely say there were metrics," said Evans. Such metrics or sales goals and quotas can include things like: number of vaccines given, number of consults given, number of student trainees taken on, and the number of automatic refills dispensed. In May, the American Pharmacists Association, or AphA, the largest professional group representing pharmacists in the United States, cited concerns over "realigning unreasonable metrics and workload."
Pharmacy techs in some cases have it even worse. At Walgreens, pharmacy tech pay will now start at $16.50 per hour, which spokesperson Fraser Engerman cited as a way the company has responded to problems with increasing staff levels and retaining existing staff. This is still below the national median pay of $17.33 per hour, which comes out to a salary of less than $40,000 per year, hardly a livable wage in many parts of the country.
Understaffing has become a larger problem throughout the pandemic, with more pharmacists and techs quitting as demands increase, leading to store closures and delays in prescription fills. Eventually, to "stop the bleeding," as Jerominski described, the big chains began offering major sign-on bonuses for new pharmacists. Walgreens has offered sign-on bonuses of as much as $75,000 and, according to Engerman, hired thousands of new pharmacists and techs since 2020.
But as Jerominski put it, "If pharmacists are being offered a job with $75,000 sign-on bonuses just to commit to a few years in that position, and [there are] still so few takers, imagine how abysmal those working conditions must be." That offer may be all the more enticing given that the average pharmacist graduates with $180,000 in debt.
Another effort Walgreens cited to improve staffing and retention was creating the new position of "pharmacy tech manager," Salem's job, which she said pays $22.50 per hour in the Chicago area. She describes the role as "a glorified tech who bosses around other techs and makes the schedule and gets yelled at for metrics."
Like many others, Salem is looking for a way out. "I am overworked, and stressed, and unhappy, and considering quitting every day. I work 10 to 20 hours of overtime per pay period, staying late and coming in early every day. My first vacation in over a year is being challenged."
There have been some efforts to fight poor working conditions: California passed a law earlier this year prohibiting pharmacies from enforcing quotas. Yet the quotas continue in most other states, though there have been a few similar efforts by state boards to cap the number of prescriptions filled per day per pharmacist. Illinois, for example, has one of the strictest laws around limiting hours for pharmacists and requiring breaks.
The end of federal funding for Covid vaccines and tests, which President Joe Biden announced in August, could mark a new era for pharmacies and for patient care. The latest vaccines are still covered by the government, but after that, it's going to get more complicated. Pharmacy billing experts will have to spend more time contending with different insurance plans, and pharmacy chains will be weighing the costs versus profits. Matt fears that as pharmacies have to buy the vaccines, corporations like CVS and Walgreens may decide they are no longer worth it. "Once that funding stops and the pharmacy chains have to buy the vaccine, it will cause a significant shift. Waste will no longer be acceptable, and some chains may go away from the Covid vaccines altogether," he said.
In the meantime, pharmacy employees are still grappling with the extra demands on their time. As Salem said, "The boosters being released on top of flu season has decimated my pharmacy. We can't help anyone anymore."
Comments
Post a Comment